A popular class of diabetes and obesity drugs may help keep certain cancers at bay, new research suggests. Scientists have found evidence that GLP-1 medications are associated with a lower risk of 10 different obesity-related cancers in people with type 2 diabetes, compared to only taking insulin. Newer, more potent GLP-1 drugs such as semaglutide and tirzepatide could provide an even greater buffer against cancer, the scientists say.
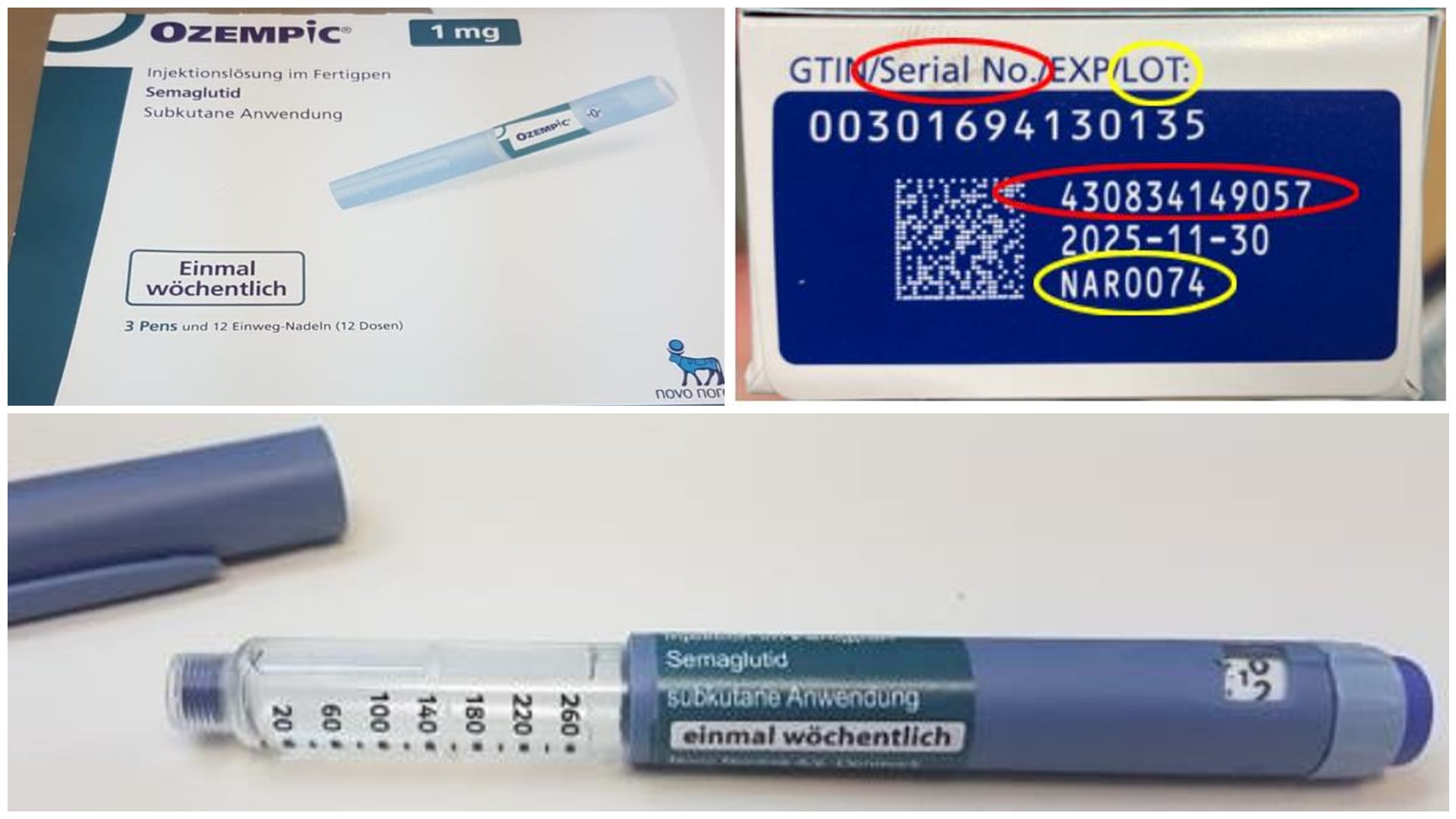
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) have been used since the early 2000s to treat type 2 diabetes. They mimic the naturally occurring hormone GLP-1, which helps regulate our metabolism by prompting the release of insulin when needed. As it turns out, the hormone also plays a role in regulating our appetite, leading to the approval of GLP-1 drugs as treatments for obesity (the first official medication in the U.S. was liraglutide in 2014). More recent drugs such as semaglutide (the active ingredient in Ozempic and Wegovy) and tirzepatide (Mounjaro/Zepbound) have proven to be substantially more effective at helping people lose weight than diet and exercise alone. In clinical trials, people using these drugs have lost an average of 15% to 20% of their body weight over a year’s time.
This new study was led by researchers from Case Western Reserve University in Ohio. They were interested in studying the health benefits of GLP-1 drugs beyond diabetes and obesity. Because obesity has been tied to a greater risk of 13 cancers, including breast, thyroid, and pancreatic cancer, the team wanted to know if the medications would provide a preventive anti-cancer effect as well. Their earlier work had suggested that GLP-1s are associated with a lower risk of developing colorectal cancer specifically. But as far as they know, this is the first research to systematically look at the link between obesity-related cancers and GLP-1 use.
The scientists analyzed medical record data from 1.6 million patients diagnosed with type 2 diabetes and no pre-existing cancer history. The team studied three subsets of patients who were prescribed different drugs to manage their diabetes sometime between 2005 to 2018: people who were prescribed a GLP-1 drug, people prescribed insulin, or people prescribed metformin, another common diabetes medication. The latter two groups acted as a sort of control comparison.
Overall, the team found that people prescribed GLP-1s had a noticeably lower risk of developing 10 out of the 13 cancers associated with cancer, including gallbladder, pancreatic, liver, and colorectal cancers, when compared to those taking insulin. GLP-1 users may also have had a lower risk of several cancers when compared to metformin users, though the differences were not statistically significant. The team’s findings were published Friday in the journal JAMA Network Open.
This sort of research can only demonstrate a correlation between GLP-1 use and cancer risk, not prove a cause-and-effect relationship. The study can’t also tell us why GLP-1s might protect us from cancer, though the researchers already have some possible explanations in mind.
“The protective effects of GLP-1 RAs against obesity-associated cancers likely stem from multiple mechanisms,” lead author Lindsey Wang, an undergraduate in Case Western Reserve University’s Pre-Professional Scholars Program (a 8-year-long program that combines a Bachelor’s and medical degree), told Gizmodo in an email. “Primarily, these drugs promote substantial weight loss, reducing obesity-related cancer risks. They also enhance insulin sensitivity and lower insulin levels, decreasing cancer cell growth signals.”
Not all the team’s findings were good news. Compared to those on metformin, people on GLP-1s did appear to have a higher risk of kidney cancer. There was also no difference in the risk of thyroid cancer between insulin and GLP-1 users. But since some evidence has found that high insulin levels in the body can raise thyroid cancer risk, that might suggest GLP-1 use can do the same. Notably, some studies in animals have found that GLP-1 drugs can increase the odds of a specific, rarer type of thyroid cancer: medullary thyroid cancer. But the evidence of this added risk in humans has been inconclusive so far.
Even if these negative cancer risks are causally linked to GLP-1 use, though, their anti-cancer benefits elsewhere should likely outweigh them, according to Wang. “The significant risk reductions, particularly for cancers with high mortality rates, indicate a net positive effect,” she explained.
Another important wrinkle is that the study mostly covered the earliest eras of GLP-1 use. The first semaglutide-based drug, Ozempic, was only approved for type 2 diabetes in 2017, for instance, while tirzepatide was first approved in 2022. Given the higher effectiveness in weight loss seen with these newer medications, it’s certainly possible that they will have an even more profound effect in preventing cancer, Wang said.
On a sadder note, study author and cancer researcher Nathan Berger passed away just this past June at the age of 83. Berger was the founding director of the Case Comprehensive Cancer Center and more recently the director of the university’s Scientific Enrichment Opportunity (SEO) & Youth Engaged in Science (YES) programs that encourage high school students to get involved in scientific research. Berger was also one of Wang’s mentors.
“I would like to attribute this study to Dr. Nathan Berger, who conceptualized and supervised this study as the senior author.” Wang said.
As exciting as the idea that these increasingly popular drugs can also help prevent cancer might be, this research is only the beginning, according to Wang. We need studies that can directly examine this possibility as well as studies that can try to figure out exactly how these drugs fend off cancer.
“Moving forward, prospective randomized clinical trials are essential to confirm these associations and establish causality. Preclinical studies are needed to elucidate the underlying mechanisms,” she said. “Additionally, research to examine the newer and more potent weight loss GLP-1RAs (semaglutide and tirzepatide) would be particularly important.”